Postoperative pain (POP) is one of the most common types of acute pain. It can be defined as an anticipated and temporary increase in background pain present in surgical patients after a procedure. It is estimated that up to 80% of patients undergoing various surgical procedures experience pain and, of those, 40 to 60% experience moderate to severe or extreme postoperative pain. With an estimated market size of USD 45 Bn in revenue by the end of 2026 driven by the continuously growing population and the increasing awareness about the surgical treatments in cancer and other chronic diseases, POP is a socio-economic issue and remains a key indication with a large patient potential.
What is Acute POP?
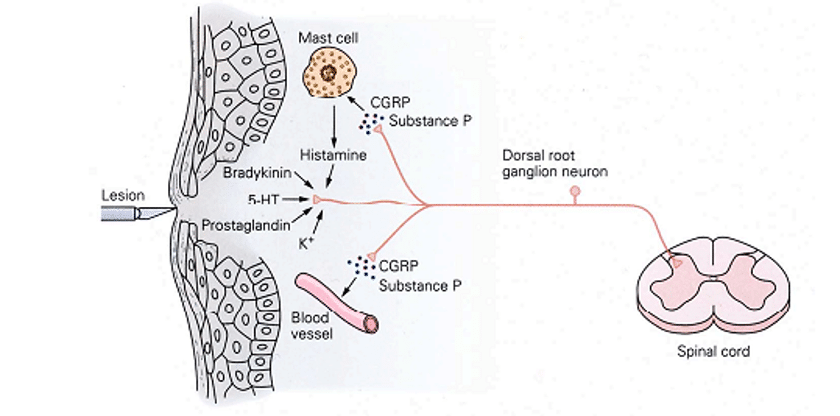
Acute POP is one of the most distressing aspects of surgery and remains considered as a mandated part of the comprehensive surgical postoperative experience. It is a complex physiological reaction to tissue injury that manifests from autonomic, psychological and behavioral responses. It is currently characterized by:
- Transient but extremely strong activation of the nociceptive network
- Impaired Quality of Life (QOL) (energy, sleep, joy in life, physical mobility, cognitive functions, emotional reactions)
- Anxiety and depressive symptoms
The clinical aspects of the sensitization are expressed as an increased pain for a given stimulus. Such “hyperalgesia” may be detrimental in the early postoperative period and may also induce stress. It is strongly linked to movement-evoked pain, against which the patient may behave by avoiding any painful movement. This strategy, however, may impact rehabilitation and prolong the patient’s hospitalization.
Since the five past decades, the treatment of POP has been relevantly improved by various factors:
- the increased knowledge about the mechanisms of pain and its sensitization
- the availability of analgesics systemically administered, such as paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs) or nefopam
- the gained popularity of opioids, with the help of patient-controlled administration (PCA)
- the development of loco-regional techniques (peripheral nerve blocks)
Appropriate pain relief has relevant effects on the patient’s general health (earlier oral feeding, less postoperative delirium, easier mobilization of the operated limbs, better spontaneous ventilation after thoracic and visceral surgeries and reduction in postoperative cardiovascular complications). Appropriate pain relief leads also to shortened hospital stays and reduced hospital costs.
POP remains a significant medical problem!

However, despite all the significant advances mentioned above, POP remains a significant medical problem. When poorly managed, POP leads to complications and prolonged rehabilitation, negatively affects QOL and increases the risk of persistent postsurgical pain with the development of chronic pain which may result in longer-term psychological, social and economic adversity.
WHAT ARE THE CURRENT TREATMENTS?
In the clinical practice, pain control generally takes place with:
Opioid Analgesia
In many settings, the mainstay of postoperative pain therapy remains opioids. They act on the spinal transmission of nociception, the cognitive perception of pain and the descending controls. They can be administered via various routes. The most commonly used intravenous opioids for postoperative pain are Morphine, Hydromorphone and Fentanyl.

Non-opioid Analgesia
Opioid-sparing techniques using different analgesic mechanisms of action is also recognized as an important component strategy for postoperative pain management.
- NSAIDs act on prostaglandin-mediated peripheral and central sensitization. They are useful in reducing the amount of opiates requested and administered to the patient thus reducing opioid side effects. They are used from mild to moderate levels of pain.
- Acetaminophen is a centrally acting analgesic (serotonergic ± endocannabinoid descending controls), but lacks peripheral anti-inflammatory effects. Oral acetaminophen represents the first-line treatment (if no contraindication) and is widely used for acute pain relief. Acetaminophen is a common ingredient in many combination oral pain medications.
- Nefopam acts centrally but its mechanism of action is still not well documented.
Finally, the loco-regional techniques, by blocking the nociceptive afferent volley (sodium channels of the fibres) are well effective on POP at movement but require a trained staff, are expensive and may represent a risk of infection.
The Future direction!
Although POP is treatable, evidence suggests that less than half of patients who undergo surgery report adequate postoperative pain relief. It remains strongly embedded in people’s minds that pain is an inevitable consequence of surgery. Other identified reasons/limitations are also:
- the underuse of available guidelines, pain assessment and written protocols
- the moderate efficacy provided by the non-opioid analgesics
- the very frequent side effects of opioids, reducing the patient-estimated interest of analgesia
- the difficulties to develop long-lasting loco-regional analgesia
So, pharma research in this specific field is very active to develop a better analgesic.
PROMISING PERSPECTIVES!
A new analgesic compound that would help to improve the whole quality of POP analgesia should either be so powerful and safe that it could replace the current treatments or, at least, be able to act as a potent co-analgesic. A relevant improvement of POP therapy would be characterized, either in a sensible reduction of the use of opioids and NSAIDs, or in a strong relief of movement-evoked POP. In both cases, such improvement would help postoperative rehabilitation and ambulation, with all the implications in terms of public health.

To reach such endpoints, the following properties for a new compound would be of interest:
- New target(s) from the available analgesics
- Co-analgesic effect: Combination of analgesic compounds that act on different sites to either potentiate analgesia or reduce the necessary dose of the analgesic drugs in order to reduce their side effects.
- Antihyperalgesic effect: The aim is to directly target on the neuronal mechanism of both central sensitization (after major surgeries) and opioid-induced hyperalgesia (OIH). The NMDA receptor antagonists are the best-known antihyperalgesic agents. The most studied agent is the general anaesthetic Ketamine, administered perioperatively at low dose. Drugs acting on sites other than NMDA receptors, such as Clonidine or Gabapentin exibit also antihyperalgesic effects.
- Potency on movement-evoked POP: Apart from loco-regional analgesia, which shows strong effects, few molecules have shown a significant effect on movement-evoked POP. Only NSAIDs may act more specifically on this aspect, although the relief remains weak.
Conclusion:
To improve quality of life and functionality, enhance activities of daily living, and reduce physiological and emotional morbidity, according to the better understanding of the epidemiology and pathophysiology of pain, specialists have focused greater attention on the multimodal pain management that should be used whenever possible. Guidelines for the treatment of postoperative pain have been developed to provide safe and effective therapies with evidence-based recommendations.
At a preclinical stage, ANS Biotech can help you in the characterization of your candidate by proposing clinically relevant in vivo models in this therapeutic area. The gold standard for POP is the Brennan Model (incisional pain).
Our validated and customized behavioral studies will help you to demonstrate the efficacy of your products before they move into the clinic.
WHAT ARE THE BENEFITS
OF WORKING
WITH ANS BIOTECH?
ANS Biotech, your partner for building step by step your preclinical package
To know more about ANS Biotech services, do not hesitate to contact us!